Summary
📉 What people think

While our optimistic readers say they have high hopes for next-generation vaccine development, articles from the spring of 2020 remind us the experts were bearish about the prospect of a Covid-19 vaccine coming to the world’s rescue any time soon.
📈 Here are the facts
On the one-year anniversary of the pandemic, more than 1.3 billion doses of the brand-new Covid-19 vaccines had been administered. The breakneck speed at which the vaccines were developed signals a new era has arrived — and puts the spotlight on the wide range of devastating diseases that the new technologies can potentially solve next. Bye, cancer?
💡 The Optimist’s Edge
Vaccine platforms, global infrastructure, and money — gobs of it. It all paved the way for the groundbreaking Covid-19 vaccines. But, perhaps, even more importantly, it created a blueprint for the future. We have seen what’s possible and can do it again, and again. That spells good news for global health — and your future wellbeing.
👇 How to get the Optimist’s Edge
No year has seen more clinical trials for mRNA-based cancer vaccine therapeutics than 2021. It is just one development brought about by the Covid-19 vaccine success that you can help support — or participate in.

📉 What people think
The lightning speed of the Covid-19 vaccine development has buoyed our readers. When asked whether they think there will be vaccines for other serious diseases, such as cancer, AIDS, and Alzheimer’s in their lifetime, as many as 7 out of 10 replied yes.
Only last year, many were likely not so optimistic.
Let’s turn back time to April of 2020. The SARS-CoV-2 pandemic was sweeping across the globe. Deaths mounted as the debate over restrictions and lockdowns raged 24/7. If only Dr. Anthony S. Fauci, the U.S. top infectious disease expert, ventured a guess. It would be 12 to 18 months — if we were lucky. The New York Times called it a “rosy forecast.”
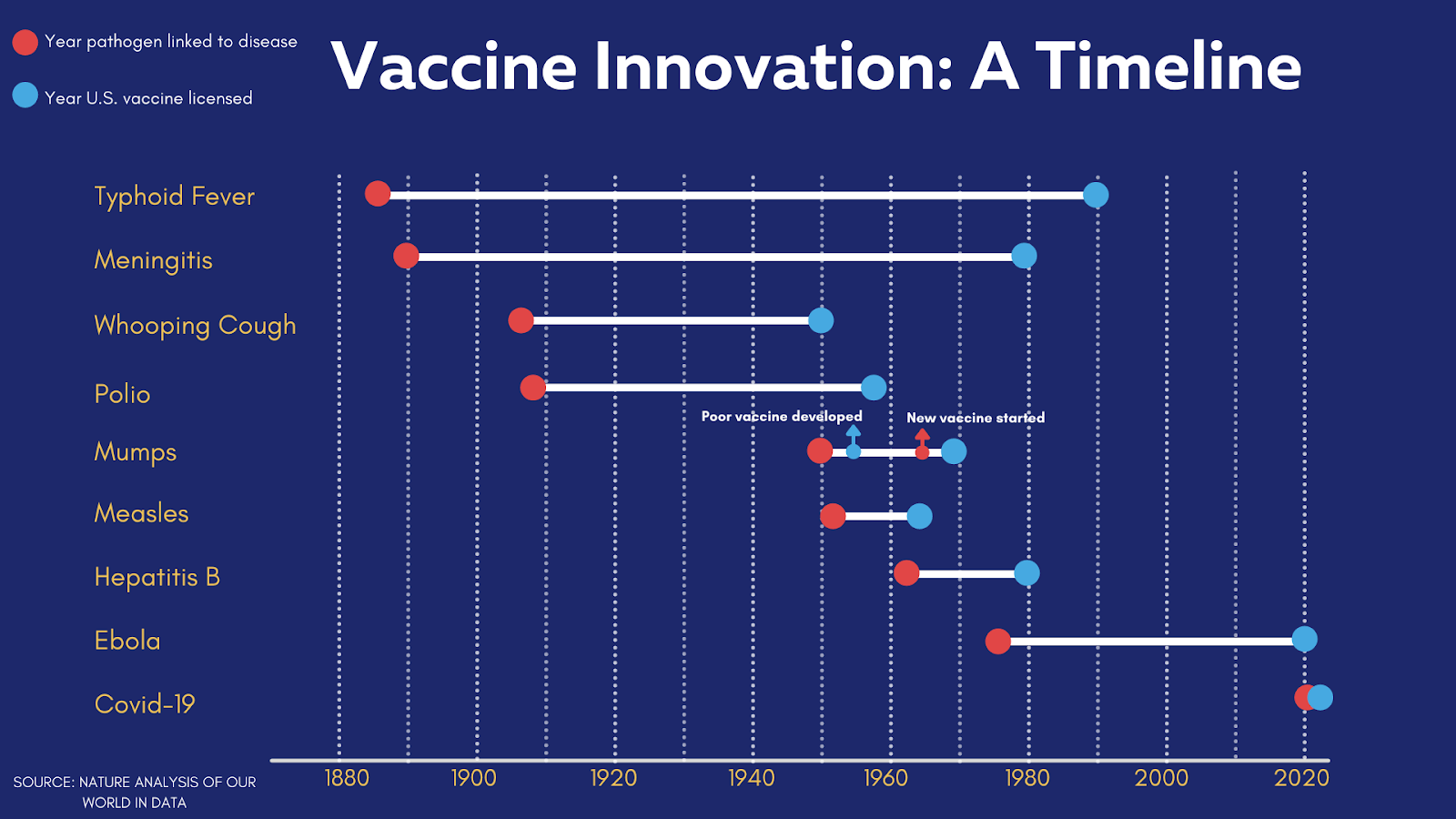
At the time, the vaccine for the mumps virus was the fastest ever developed; in the 1960s, it took four years from virus sampling to approval. Other vaccines had typically taken a decade or longer. The chickenpox vaccine development churned for 28 years, the rotavirus and human papillomavirus both clocked in at 15 years. In the most dire scenario, the NYT estimated the world would have to wait until 2033 for a Covid-19 vaccine.
“The grim truth,” the NYT wrote, “is that a vaccine probably won’t arrive any time soon. Clinical trials almost never succeed. We’ve never released a coronavirus vaccine for humans before… “But if there was any time to fast-track a vaccine. It is now.”
📈 Here are the facts
About 12 months after the publication of the NYT article, the success of the Covid-19 vaccine development exceeded even the rosiest forecasts. As the pandemic reached the one-year mark, more than 1.3 billion vaccine doses had been administered and three vaccines enjoyed emergency-use authorization (EUA).
Most of us can remember the feeling of awe when we learned Moderna’s RNA vaccine had entered clinical trials only two months after researchers sequenced the SARS-CoV-2 genome in January of 2020. If the pandemic had struck only five years earlier, experts say the innovative RNA technology would not have been ready.
Once upon a time
The story of the Covid-19 vaccines and the record pace at which they were developed began decades ago. Little did the researchers of the 1980s know that their work to create adenoviral vectors would lead to the sensational development of our first Ebola vaccine as well as two pandemic game changers, the vaccines from AstraZeneca and Johnson & Johnson.
And no one could have imagined the significance of a 1988 chance meeting at a Xerox machine of two scientists at the University of Pennsylvania. After a brief exchange about taking turns on the copier, Drew Weissman told Katalin Karikó that he was using DNA to make an HIV vaccine. She argued for RNA. They decided to collaborate.
In 2005, they published a landmark research paper that explained how messenger RNA, or mRNA, could be altered for therapeutic use. Now, their modified mRNA technology is licensed by Moderna and Pfizer/BioNTech and constitutes one of several groundbreaking developments that have not only helped turn the tide on the pandemic but also offer promise for combatting a range of deadly diseases.
Ready, set, research
Three years before the pandemic hit, Moderna, for example, built a $130 million, two-storey manufacturing plant in Norwood, Mass., to synthesize and formulate mRNA for the company’s early-stage clinical trials, including an ongoing investigation of a personalized cancer vaccine. The application of mRNA, it had been discovered, can train the immune system to recognize and destroy disease-causing agents, be they cancer cells or infectious viruses.
It’s the human version of plug-and-play — and the possibilities are potentially endless.
Diseases that have proved impervious to conventional vaccines are now the target of mRNA technology, including viruses such as cytomegalovirus (CMV), a common infectious cause of neurological defects in newborns, and respiratory syncytial virus (RSV), a potentially serious airway inflammation that can land babies and young children in the hospital.
Neurodevelopmental disorders such as ALS and dementia; genetic conditions like sickle-cell anemia; infectious diseases like Lyme and herpes; and parasitic diseases like malaria, hookworm, and leishmaniasis — there may finally be an end or relief in sight for the suffering they cause.

In early 2021, a patent for an RNA-based vaccine against malaria was indeed approved. Richard Bucala, the vaccine’s co-inventor and a scientist at the Yale School of Medicine, told The Atlantic:
“We’ve been working on this vaccine for years, but the entire landscape has changed in the last six months because of the success of COVID vaccines.”
A little more than a year earlier, only months before news seeped out from Wuhan, China, about a novel coronavirus, Nature noted — prophetically — researchers can take advantage of “the [mRNA] platform’s ease of manufacture to create rapid-turnaround products.”
💡 The Optimist’s Edge
The pandemic has become a catalyst for skyrocketing investments in vaccine research. Investors have, historically, had a lukewarm interest in funding vaccine development. The return on investment has been perceived to be low, especially when an illness is not spreading like wildfire. That all changed overnight when governments, philanthropic organizations, and investors sent Covid-19 vaccine development into overdrive with an unprecedented infusion of funds.
Although investing at risk is not a new concept in drug development, the pandemic brought the phenomenon to the extreme. McKinsey, the global consulting firm, observed, “Now that they have seen the levels of acceleration achieved, companies should feel emboldened to invest at risk in other priority programs that merit the attention — for instance, in transformative therapies that can address unmet medical needs.”
Countdown to takeoff
When funds poured in, pharmaceutical companies, in turn, stood ready to capitalize on the infrastructure, platforms, and lessons learned from the fight against other virus outbreaks like MERS, Ebola, and Zika. The Coalition for Epidemic Preparedness Innovations (CEPI), for example, launched in 2017 to create a technological framework to enable speedy and affordable development of vaccines.
This dynamic shows the Covid-19 vaccine success was hardly a stroke of luck but the blueprint for future pandemics and next-generation vaccine research. In fact, human vaccinology could make a quantum leap, a high-profile virologist told Nature, as a result of all the data gathered between now and the start of the pandemic. And the next round of innovation should not have to cost as much as the Covid-19 bonanza.
“RNA simplifies the manufacturing a lot,” the chief scientist at GlaxoSmithKline’s Vaccines Division observed. “You can use the same facility to make RNA for different diseases. That decreases the investment required.”
For Covid-19 alone, there are, as of this writing, an additional 128 Covid-19 vaccine candidates in clinical trials and 194 in preclinical development.
👇 How to get the Optimist’s Edge
What’s in it for you?
The vaccine revolution presents a smorgasbord of opportunities. Take your pick.
Donate
None of the above happened overnight. And none of it happened for free. Gavi, for example, is a global vaccine alliance that brings together public and private sectors to fulfill its mission of increasing the equitable and sustainable use of vaccines. Since its inception in 2000, Gavi has contributed to the vaccination of 888 million children. A $5 donation buys one vaccine.
Invest
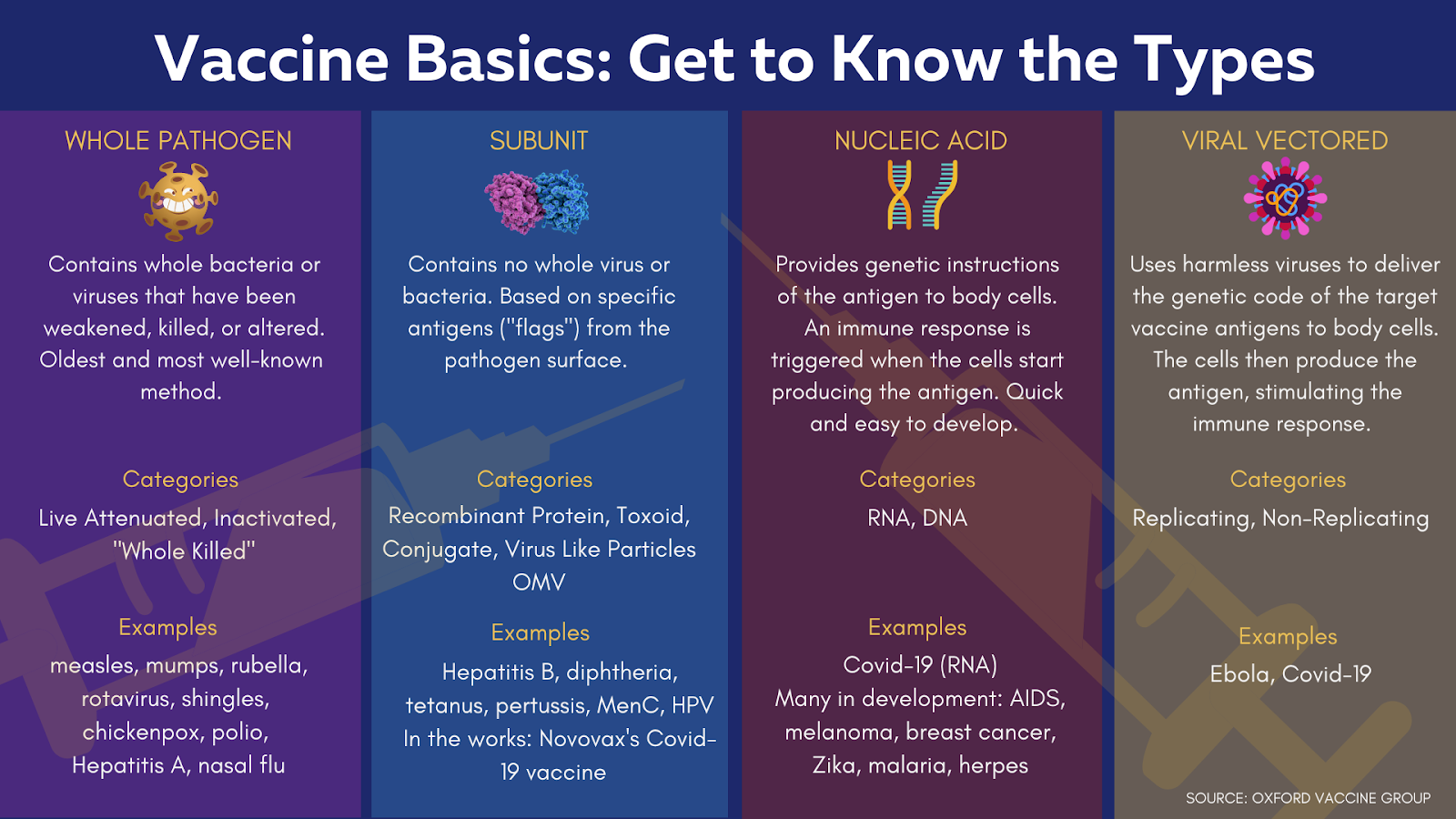
What vaccine technology holds the most promise? Viral vectored, recombinant, RNA, or DNA plasmid, which, like RNA, is a nucleic acid vaccine that has so far only seen veterinary uses but is more stable than RNA at higher temperatures and therefore of great interest. Or, is another Moderna-like success story waiting in the wings with a different solution altogether?
While the big players currently hog the global spotlight, the large number of vaccine candidates and treatments in progress proves the field is more diverse than it may appear.
Flagship Pioneering, the venture capital firm that launched Moderna, recently poured $50 million into Laronde, an early-stage biotech startup. Laronde creates eRNA, or endless RNA, that the company describes as more stable than mRNA and an “emerging class of programmable medicine.”
Another biotech startup, Atalanta Therapeutics, has this year raised $110 million for its pioneering treatment options for neurodegenerative diseases. Using a proprietary platform for RNA interference (a Nobel prize-winning discovery), Atalanta is initially focused on therapeutic treatments for Alzheimer’s, Huntington’s disease, and Parkinson’s disease.
The vaccine revolution is also fueling an ecosystem of suppliers, manufacturers, and specialized logistics companies. If this sector was on the rise before the pandemic, growth is now accelerating.
Companies like West Pharmaceutical Services (maker of packaging components and delivery systems for injectable drugs), Catalent Inc. (delivery technologies for drugs and biologics), Corning, Inc. (vial manufacturer), and Germany’s Evonik Industries AG (lipids supplier), all thrive along the vaccine supply chain. Even as the vaccines rapidly evolve, investment advisers point out this ecosystem tends to keep humming since the need for supplies largely remains stable.
Monitor
Catch an infection before symptoms surface. This is the goal of a research team at Stanford University which partnered with wearable manufacturers Fitbit and Garmin to track the biometrics of participants just as the pandemic began. Interestingly, by February of 2021, the project had successfully detected early stages of Covid-19 in 70 percent of observed cases and notified them using a consumer-friendly mobile app.

Participate
If you or someone you know is battling a serious disease, you are likely trying to stay on top of the latest research and any experimental treatments. The silver lining of the pandemic is a significant increase in mRNA-based clinical trials, such as vaccine therapeutics for cancer. The National Cancer Institute lists clinical trials that use the personalized cancer vaccine mRNA-4157.
And Moderna, for instance, is currently recruiting for a range of trials, including human metapneumovirus (hMPV), CMV, seasonal influenza, Zika, and Methylmalonic Acidemia, a genetic disorder.
Go to work
Another strain or virus will inevitably emerge. If you want to take a hands-on approach, Stanford and others offer professional certificates in, for example, genetics and genome. Or, you can go all the way and embark on a career in the field. Clinical research professionals were in short supply before the pandemic and demand is now higher than ever. Next time we write an article on human health and biology, you may be the real expert.
Read more
This 52-year-old sales rep in Massachusetts received an experimental mRNA cancer vaccine for melanoma.
The world’s most powerful drug factory may be inside all of us — a story on mRNA.
What more can you do?
Please share more ideas with your fellow Premium Supporters in our Facebook group.
Captions
mRNA1: The mRNA encodes a key protein of SARS-CoV-2 inside our cells.
mRNA2: Messenger RNA (red) produced from a DNA strand.
CovidVaccine: What’s next for Covid-19 vaccine technology?
Vaccine1: Gavi, a global vaccine alliance, has contributed to the vaccination of 888 million children.
Vaccine2: Since the pandemic began, 7.2 billion doses have been given worldwide.
Warp_Vaccine Stats: The pace of development of the Covid-19 vaccines was unlike anything the world had seen before.
Stats
Annual Deaths Worldwide:
- Cancer: 9.5 million
- Malaria: 409,000
- Alzheimer’s: 819,000
The number living with disease:
- Alzheimer’s: 44 million
- Sickle-Cell: Around 100 million
- ALS: Around 6,000 are diagnosed every year in the US.





